Abstract
Introduction: Cytogenetics remains one of the most important prognostic factors in acute myeloid leukemia (AML) patients, even for outcomes after allogeneic hematopoietic cell transplantation (allo-HCT). Complex karyotype (CK) constitutes a cytogenetic category with a very adverse prognosis in this setting. However, CK is a heterogenous and loosely defined category which comprises a high diversity of cytogenetic subtypes, which is highly enriched with specific cytogenetic subtypes characterized by losses of chromosomal material at critical regions known to confer a poor prognosis per se, such as monosomal karyotype, del(7q)/-7, del(5q)/-5 or abnormalities leading to 17p region loss. On the contrary, rare AML cases characterized with only multiple numerical abnormalities known as pure hyperdiploid karyotype (HDK), have a controversial prognosis. We hypothesized that pure complex HDK AML has a distinct and much better prognosis after allo-HCT compared to non-HDK, CK AML.
Methods: We selected from the EBMT registry adult patients with AML and a full cytogenetic report. HDK was defined by the presence of 49 chromosomes or more. Patients were then stratified by pure HDK (pHDK) and HDK with other cytogenetic abnormalities (HDK+), characterized by HDK and the presence of a prognostic-defining cytogenetic abnormality such as del(5q)/-5, del(7q)/-7, del(17p)/-17/i(17q), inv(3q21-26)/t(3;3)(q21;q26) or t(9;22). We included only first allo-HCT from a sibling or unrelated donor (UD) performed between 2000 and 2018.
Results: A total of 236 patients were identified as having HDK. There were 95 pHDK and 141 HDK+. Median age at transplantation was 53 years (range, 18-74) and median follow-up was 43 months (range, 35-56). A diagnosis of secondary AML was reported in 48 patients (20%). At the time of allo-HCT, 180 patients (76%) were in first remission (CR1), and 56 were beyond CR1 (24%). Eighty-five (39%) patients received an allo-HCT from a sibling donor, with more matched unrelated donors (MUD) in HDK+ patients (p=0.02). Most patients (70%) had a Karnofsky performance status (KPS) score of more than 90% at the time of transplantation. A myeloablative conditioning regimen was administered in 46% of the patients. In vivo T-cell depletion was part of the regimen in 66% of the patients. The most frequent trisomies were trisomy 8, 21, 13, and 22.
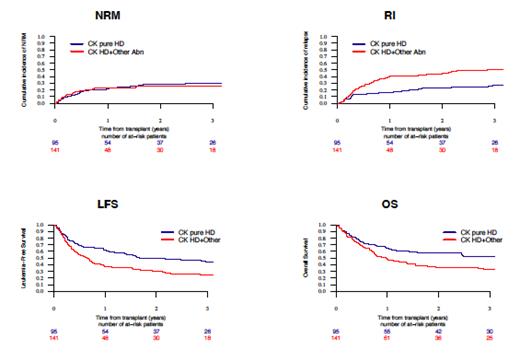
The 2-year probability of non-relapse mortality (NRM) was 26% for the entire cohort. The 2-year probability of LFS was 50% for pHDK and 31% for HDK+ (p=0.003). The 2-year probability of overall survival (OS) was 57% for pHDK and 36% for HDK+ (p=0.007). The 2-year cumulative incidence of relapse (RI) was 22% for pHDK and 44% for HDK+ (p=0.001) (Figure 1). The cumulative incidence of grade II-IV acute graft-versus-host disease (GvHD) and chronic GvHD was 34% and 33%, respectively, for the entire cohort. Finally, the 2-year probability of GvHD and relapse-free survival (GRFS) was 36% for pHDK and 21% for HDK+ (p=0.01). On multivariate analysis, pHDK remained associated with significantly better LFS, OS and GRFS and higher RI (all p-values<0.004). Age was associated with lower OS (p=0.05). Being in remission at the time of allo-HCT was associated with better LFS, OS and GRFS, and lower NRM and RI (all p-values<0.02). Secondary AML, donor type, KPS, and conditioning regimen intensity were not associated with any outcome in multivariate analysis.
Conclusions: AML with pHDK has a better outcome after allo-HCT in terms of RI, LFS, OS and GRFS. pHDK AML constitutes probably a distinct cytogenetic entity from HDK+ or other non-hyperdiploid CK AML. CK remains a strong indication for allo-HCT, but the type of abnormalities included in CK significantly influences the outcome and should guide how to manage patients after allo-HCT in terms of immunosuppression withdrawal or prophylactic/preemptive post-transplant interventions such as use of hypomethylating agents or donor lymphocyte infusions.
Labopin: Jazz Pharmaceuticals: Honoraria. Ganser: Jazz Pharmaceuticals: Honoraria; Novartis: Honoraria; Celgene: Honoraria. Socie: Alexion: Research Funding. Forcade: Novartis: Other: travel grant. Chalandon: Incyte, BMS, Pfizer, Abbie, MSD, Roche, Novartis, Gilead, Amgen, Jazz, Astra Zenec: Other: Travel EXpenses, Accomodation; Incyte, BMS, Pfizer, Abbie, MSD, Roche, Novartis, Amgen: Other: Advisory Board; Incyte: Speakers Bureau. Yakoub-Agha: Jazz Pharmaceuticals: Honoraria. Kröger: Novartis: Research Funding; Riemser: Honoraria, Research Funding; Sanofi: Honoraria; Neovii: Honoraria, Research Funding; Jazz: Honoraria, Research Funding; Gilead/Kite: Honoraria; Celgene: Honoraria, Research Funding; AOP Pharma: Honoraria. Esteve: Jazz: Consultancy; Bristol Myers Squibb/Celgene: Consultancy; Abbvie: Consultancy; Novartis: Consultancy, Research Funding; Astellas: Consultancy; Pfizer: Consultancy; Novartis: Research Funding. Mohty: Sanofi: Honoraria, Research Funding; Pfizer: Honoraria; Novartis: Honoraria; Takeda: Honoraria; Jazz: Honoraria, Research Funding; Janssen: Honoraria, Research Funding; Gilead: Honoraria; Celgene: Honoraria, Research Funding; Bristol Myers Squibb: Honoraria; Astellas: Honoraria; Amgen: Honoraria; Adaptive Biotechnologies: Honoraria.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal